Early Intervention and Rehabilitation Centre for Children in Mumbai, India: A Journey from Diagnosis to Rehabilitation
By Dr Prerna Khar1, Dr Vinyas Nisarga2, Dr Swati Shelke2, Dr Henal R Shah3, Dr Surbhi Rathi4
1Consultant, Department of Psychiatry, Early Intervention and Rehabilitation Centre for Children, TNMC and BYL Nair Ch. Hospital, Mumbai, India
2Assistant Professor, Department of Psychiatry, Early Intervention and Rehabilitation Centre for Children, TNMC and BYL Nair Ch. Hospital, Mumbai, India3Professor (Additional), Department of Psychiatry, Coordinator, Early Intervention and Rehabilitation Centre for Children, TNMC and BYL Nair Ch. Hospital, Mumbai, India
4Professor & Head, Department of Paediatrics, Coordinator, Early Intervention and Rehabilitation Centre for Children, TNMC and BYL Nair Ch. Hospital, Mumbai, India
Introduction
In India around 11 million children in the age group of less than five years are affected by developmental disorders as per the Global Burden of Disease survey.1 The age group of 10-19 years contributes to the highest percentage of disability which is 17%, and 1.2% belong to the age group of 0-6 years.2 Unfortunately, fewer than 1% of children and adolescents are able to get treatment for their mental health in India.3 Sourander A et al. (2018) reported that India had just 0.02 child and adolescent psychiatrists for every 100,000 children aged 14 years or younger.4 The numbers drop down further for children with neurodiversity or disabilities. Research has time and again reiterated that interventions provided at the early stages of development have proven to be extremely effective in catering to developmental challenges of children with special needs, thereby enhancing their quality of life.
Conception of the Early Intervention and Rehabilitation Centre for children (EIRCC), Mumbai
Around 6% of children are born with birth defects, and 10% face developmental delays, which can lead to permanent disabilities without timely intervention.5 To address this, the Ministry of Health and Family Welfare, Government of India launched the ‘Child Health Screening and Early Intervention Services’ under the National Rural Health Mission, establishing District Early Intervention Centres (DEICs) for children aged 0-6 years.6-11
Very few District Early Intervention Centres (DEICs) have been allotted to the state of Maharashtra, which mostly provide services to children only in the age group of 0-6 years. Though the district of Mumbai has a huge population, there is no DEIC to cater to neurodiverse children. Thus, the Early Intervention and Rehabilitation Centre for Children (EIRCC) was started by the Municipal Corporation of the city of Mumbai. Affiliated to B.Y.L. Nair Charitable Hospital and Topiwala National Medical College, Mumbai, this facility not only provides rehabilitation but also offers research and training opportunities, setting a benchmark for other DEIC centers. The EIRCC is an all-inclusive centre delivering a broad spectrum of evidence-based therapies, interventions, and support services to children facing developmental challenges and disabilities.

Figure 1: Early Intervention and Rehabilitation Centre for Children
The centre, housed in five-storeyed building spanning 35,000 square feet, was proposed in 2018, with the first phase completed in 2023. Catering to children from 0 to 18 years of age, EIRCC provides its services entirely free of cost, ensuring accessibility to early intervention and rehabilitation support. Each floor of the building is designed with a unique child-friendly theme, creating a soothing and engaging environment to make the experience comfortable and less intimidating for children. Currently, the team includes a Pediatric Neurologist, Neurodevelopmental Pediatrician, three Child Psychiatrists, two Pediatric Ophthalmologists, two ENT specialists, five speech therapists, seven occupational therapists, seven physiotherapists, three special educators, five psychologists, three dentists, two Orthopedicians, and two community developmental officers, all having additional training in working with children and adolescents with special needs.
By employing an integrated, interdisciplinary, and multidisciplinary approach, the center ensures that each child receives well-coordinated, comprehensive, and personalized care that addresses their unique needs holistically. Unlike other DEICs that typically serve children aged 0–6, this facility offers free rehabilitative services to children with special needs from birth to 18 years, following referrals from various hospitals, health centres and private clinicians.
The entire center is designed in order to be child and disability friendly. It operates on a stratified step-care model and stands apart from public hospitals by focusing on quality over quantity, allocating between 45 minutes to one hour per session. With all therapies provided under one roof, it serves as a one-stop destination for families seeking comprehensive care.
As of February 2025, the center has provided support to approximately 2,500 children with special needs, delivering around 45,000 specialized therapy sessions tailored to their requirements. In its second phase, plans include introducing additional services such as aqua-therapy, gait analysis lab, animal-assisted therapy, BERA testing, telemedicine support for remote centers, remedial education for children with learning disabilities, and an auditorium for therapy programs and specialist training. These enhancements have been approved by the Municipal Corporation of the city, with the necessary budget allocated, and are expected to be completed within the next year.

Figure 2: Physiotherapy Department @ EIRCC

Figure 3: Occupational Therapy Department @ EIRCC
Function of various departments at EIRCC (Table 1)
- Paediatric Department: Screening, assessment, diagnosing and treatment of developmental delays, seizures, neurological, neuromuscular, and genetic disorders.
- Audiology and Speech Therapy Department: Assessment and management of speech, language, communication, fluency and articulation difficulties, Oro-sensory and Oro-motor deficits, feeding and swallowing difficulties and screening of hearing and audiological testing.
- Occupational therapy Department: Assessment and management of neurodevelopmental and sensory integrative dysfunction. Assessment for orthotic, splintage and adaptive devices and training in activities of daily living. Focuses on improving fine and gross motor skills, sensory processing, co-ordination and attention span.
- Physiotherapy: Assessment & management of posture, balance, co-ordination, range of motion, muscle tone and muscle strength. Training for gait, motor skills and pain relief.
- ENT Department: Screening of hearing loss and management of various ENT disorders such as chronic/ recurrent ear infections, hearing loss, speech delays, nasal congestion, tongue tie, tonsil pathologies and respiratory issues, which are common in children with special needs.
- Ophthalmology Department: The department conducts visual screening, assessments and manages refractive errors, glaucoma, and cataracts. It provides therapy for binocular vision issues, amblyopia, and strabismus. Evaluation for orthoptics and offers low vision aids to enhance visual function for children with special needs.
- Dental Department: Addresses issues related to teeth, gums and oral hygiene offering complete orofacial prevention, restorative and surgical treatment such as dental filling, root canals, crowns, replacement of teeth.
- Orthopaedics Department: Specialized assessment and management of bone defects, fractures, and disorders in children with special needs. Correctional surgeries for bone and spinal deformities, treatment of clubfoot, bone injuries, joint infections, neuromuscular disorders, and limb malformations. Tailored care to address the unique orthopaedic needs of children with disabilities, ensuring better mobility and quality of life
- Community Development Officers: They play a key role in facilitating social interventions, enrolling special needs children in government schemes, providing guidance on financial support for their families, and fostering integration of special needs children in the community.
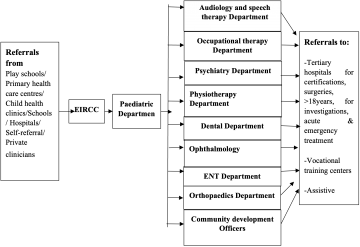
Table1: Flowchart outlining the process of flow of children and young people in the centre
Functioning of the Department of Psychiatry at EIRCC
The Psychiatry Department at EIRCC, Mumbai, India, provides comprehensive assessment and management for children with special needs in a holistic manner, using a stratified stepped care model emphasizing right care from the first time. Upon visiting, a Psychiatrist screens for emotional, cognitive, behavioral, and psychological issues, with reassessment of neurodevelopmental disorders to prevent misdiagnosis due to underlying behavioural or psychiatric issues. The child is then referred to a clinical psychologist for psychological evaluations, including assessment of caregiver burden and the parent-child relationship. After completing the assessments, the child and parents receive care from either the same psychiatrist or a counseling psychologist for management through medications and therapy. Additionally, the child is referred to a special educator for assessment, development of an individualized education plan, and to support the child's educational progress.
Weekly meetings are held to review treatment progress, address any challenges, discuss further referrals, and plan for the weaning or discontinuation of treatment. Collaboration occurs with the child's school and local therapists or clinicians (if applicable) to ensure everyone is aligned with the management plan. Parents of children with ADHD, autism, and intellectual disabilities are offered parent management therapy sessions to assist them in managing their children more effectively, while also assessing and addressing caregiver burden. Parent-child interactions are evaluated and parents encouraged to enhance attachment through parent-child interaction therapy. Additionally, group therapies have been started for children with ASD and ADHD to enhance their social, emotional and play skills. For children and adolescents requiring acute care, admission, disability certification, or care after turning 18, referral to a tertiary parent hospital is arranged.



Figure 4-6: Department of Psychiatry @ EIRCC
Conclusion
India, previously focused on acute management, is now gradually moving towards early intervention and prevention, along with rehabilitation, in Psychiatry and other medical fields. As one of the few public-sector centres in India, EIRCC serves as a model for training specialists and guiding similar centres. Two more centres are being developed in Mumbai, but given the country’s population burden, expanding such facilities with trained specialists is crucial. Tertiary care centres can play a key role by establishing and supervising these centres, ensuring administrative support, and advancing research in the field.
References
- Ansari, H. (2021). Magnitude of Developmental Disabilities in India. In: Kar, A. (eds) Birth Defects in India. Springer, Singapore. https://doi.org/10.1007/978-981-16-1554-2_7
- Pattnaik S, Murmu J, Agrawal R, Rehman T, Kanungo S, Pati S. Prevalence, pattern and determinants of disabilities in India: Insights from NFHS-5 (2019–21). Frontiers in Public Health. 2023 Feb 27; 11:1036499.
- Kommu JV, Jacob P. Specialty training in child and adolescent psychiatry in India. European Child & Adolescent Psychiatry. 2020 Jan; 29:89-93.
- Sourander A, Chudal R, Skokauskas N, Al-Ansari AM, Klomek AB, Pornnoppadol C et al (2018) Unmet needs of child and adolescent psychiatrists among Asian and European countries: does the Human Development Index (HDI) count? Eur Child Adolesc Psychiatry 27(1):5–8
- Operational guidelines RSBK-- Operational Guidelines 2013; Rashtriya Bal Swasthya Karyakram, Child health screening and early intervention services under NRHM by Ministry of Health and Family Welfare, Government of India, February 2013.
- DEIC Operation Guideline 2014: Setting up District Early Intervention Centre; Rashtriya Bal Swasthya Karyakram (RBSK), Child health screening and early intervention services Ministry of Health and Family welfare, Government of India, May 2014.
- Gafurjiwala SM, Kumar Y, Nirupama AY. Assessment of district early intervention centres in India. International Journal of Community Medicine and Public Health. 2023 Oct;10(10):3938.
- Mehta A, Khapre M, Saxena V, Martolia KS. Evaluation of District Early Intervention Centers under Child Health Screening and Early Intervention Services in Garhwal Region of Uttarakhand, India. International Journal of Health Systems and Implementation Research. 2022 Jul 22;6(1):6-13.
- Parmar, Sachin & Raghunath, Dr & Dixit, Dr & Sb, Bansal & Patidar, Dr. A cross-sectional study to evaluate the functioning and infrastructure of DEIC, and client satisfaction Ujjain and Indore districts established under RBSK.IOSR Journal of Dental and Medical Sciences. 15. 92-94.
- Rameshbabu B, Kumaravel KS, Balaji J, Sathya P, Shobia N. Health conditions screened by the 4Ds approach in a District Early Intervention Centre (DEIC) under Rashtriya Bal Swasthya Karyakram (RBSK) program. Pediatric Oncall Journal. 2019 Jul 5;16(3):73-8.
- Prabhu SA, Shukla NK, Roshni MS. Rapid assessment of rashtriya bal swasthya karyakram program implementation and beneficiary feedback at two district early intervention centers in Chhattisgarh State in India. Curr Med Issues 2021;19:3-7.
- Operto FF, Smirni D, Scuoppo C, Padovano C, Vivenzio V, Quatrosi G, Carotenuto M, Precenzano F, Pastorino GMG. Neuropsychological Profile, Emotional/Behavioral Problems, and Parental Stress in Children with Neurodevelopmental Disorders. Brain Sci. 2021 Apr 30;11(5):584.
- Hysing M, Elgen I, Gillberg C, Lie SA, Lundervold AJ. Chronic physical illness and mental health in children. Results from a large‐scale population study. J Child Psychol Psychiatry 2007;48:785–92.
- Kaptein S, Jansen D, Vogels A, Reijneveld S. Mental health problems in children with intellectual disability: use of the Strengths and Difficulties Questionnaire. J Intellect Disabil Res 2007;52:125–31.
- Lavigne JV, Faier-Routman J. Psychological adjustment to pediatric physical disorders: a meta-analytic review. J Pediatr Psychol 1992;17:133–57.
- Thurston S., Paul L., Loney P., Ye C., Wong M., Browne G. Associations and costs of parental symptoms of psychiatric distress in a multi-diagnosis group of children with special needs. J. Intellect. Disabil. Res. 2011;55:263–280.
This article represents the view of its author(s) and does not necessarily represent the view of the IACAPAP's bureau or executive committee.